What is dementia?

Dementia is not a single disease, but an umbrella term describing a collection of symptoms from a range of conditions that cause parts of the brain to deteriorate progressively. Dementia affects functions such as memory, perception, behaviour, language, and personality.
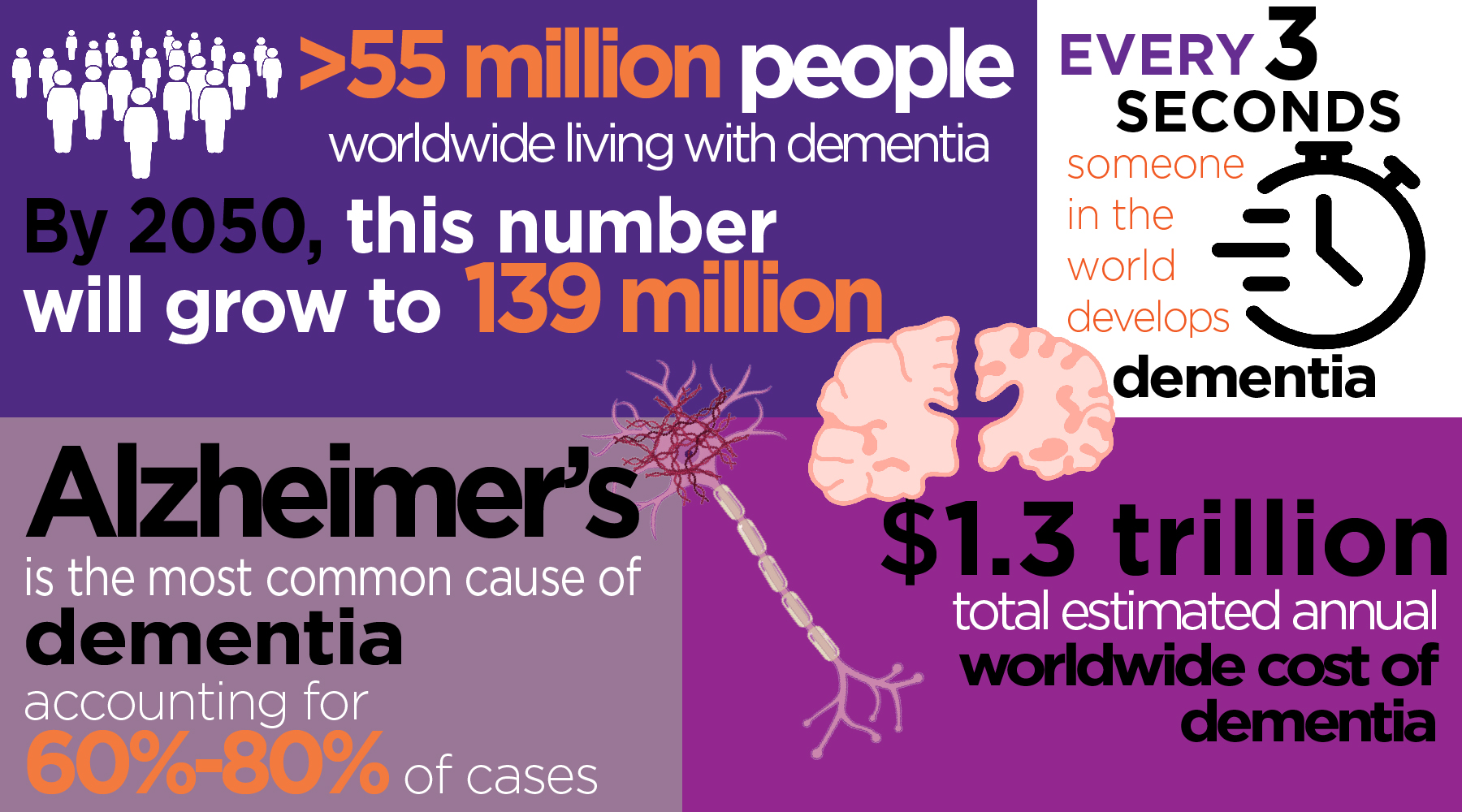
There are more than 50 conditions known to cause the symptoms of dementia. Alzheimer’s disease is the most common, accounting for about 60-70% of cases. Other common types are vascular dementia, frontotemporal dementia, and dementia with Lewy bodies. Huntington’s disease, and prion diseases like mad cow, as well as stroke, head injuries and disorders of excessive alcohol consumption can also cause dementia.
The story is further complicated by the fact that about a third of people with dementia have more than one underlying cause. As age increases, having combined forms or ‘mixed dementia’ becomes more common.
Ageing dementia is one of the country’s most pressing health problems. Alzheimer’s affects more than two-thirds of dementia patients, and approximately a quarter of a million Australians. The total number of dementia cases in Australia is expected to rise to close to 1 million by 2050. It presents significant challenges to the health care system, which makes directed research programs aimed at preventing and treating ageing dementia all the more urgent.
There is currently no cure for any form of dementia.
Who gets dementia?
- Australians with dementia in 2022:
- 401, 300 Australians are living with dementia
- 1 in 12 Australians aged 65 and over has dementia, and 2 in 5 Australians over the age of 90 have dementia
- Dementia is the leading cause of death in Australians over the age of 65.
- Dementia is the 2nd leading cause of death in Australia and the leading cause of death for women
- 28,400 Australians under 65 have younger onset dementia
- Dementia is the 5th leading cause of death in Aboriginal and Torres Strait Islander people aged 65 and over
- In the current landscape, by 2058, 849, 300 Australians will have dementia
- Cost of dementia to the Austalian economy in 2019:
- Costs of health and aged care spending directly attributable to dementia $3 billion
- When co-existing conditions are included, many of which may be directly assoicated with dementia, these health and aged care costs increase to $9.8 billion
- Carers in 2022:
- Between 137,600 and 354,200 informal carers (providing consistent unpaid care for someone with dementia)
- 75% of carers are female
- 50% of these informal carers are caring for their partner with dementia

