Motor neurone disease (MND) is an incurable and rapidly progressing disease, but researchers at The University of Queensland are testing a promising treatment option.
Professor Elizabeth Coulson, from the UQ School of Biomedical Sciences and the Queensland Brain Institute (QBI) says targeting a candidate protein has led to positive results in mice with MND.
“We’ve had encouraging positive results in MND mice, showing that we could keep dying motor neurons alive for longer and delay disease onset,” Professor Coulson said.
Protein p75 a potential drug target
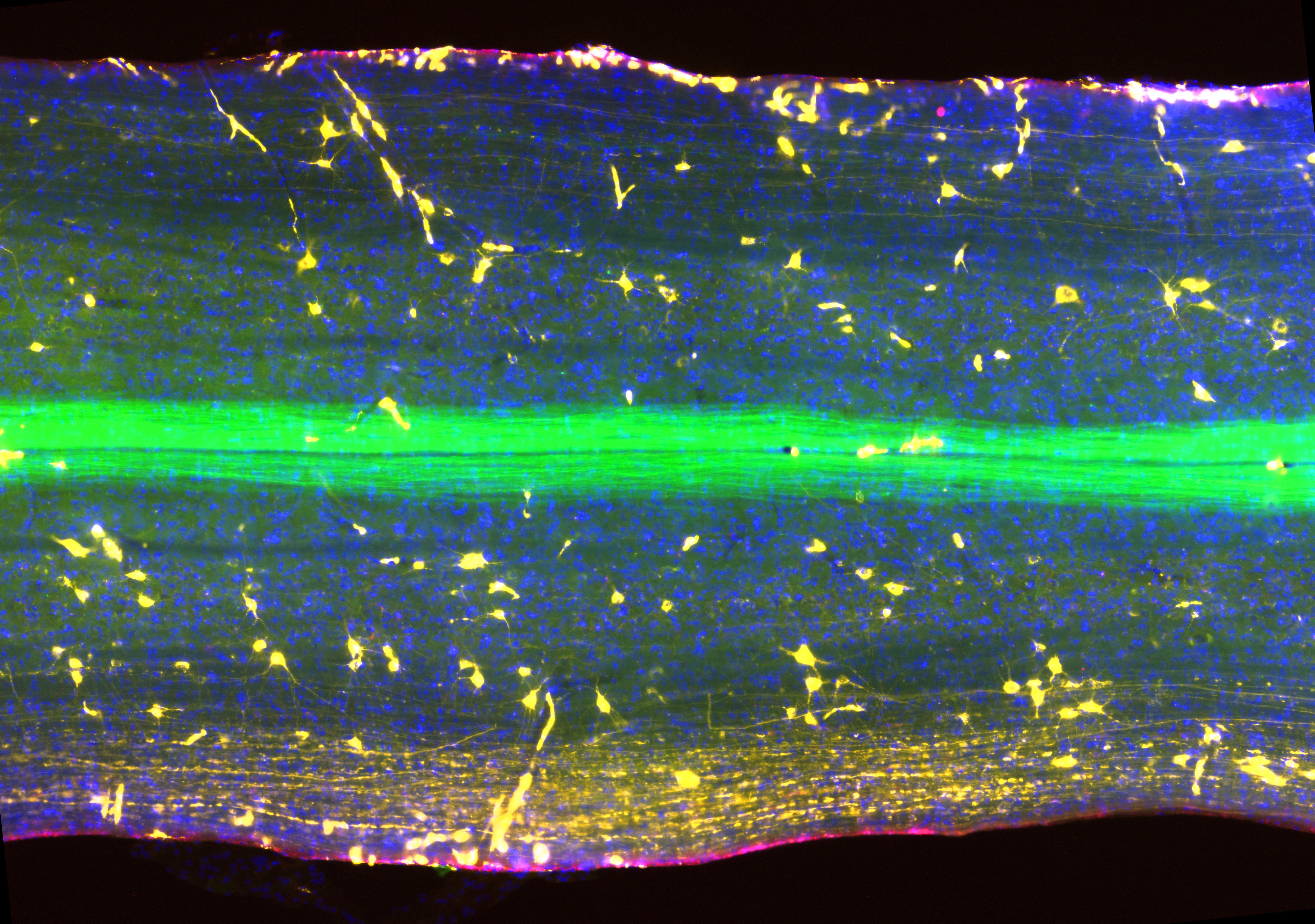
The team investigated the role of a particular protein, called p75, and its link to MND.
Professor Coulson said they blocked a cell death-signal pathway that is used by the p75 protein to kill dying motor neurons.
Collaborators from the University of Adelaide found that a by-product of this protein was found in high levels in people with MND, and could be measured in urine and blood.
Professor Coulson said mice that received treatment showed less of this by-product, indicating that motor neuron degeneration was not occuring to the same extent.
“The drop in by-product output validates investigating p75 not only as a drug target, but also as a marker for the extent of motor neuron degeneration," she said.
Applications for neurodegenerative disease
Professor Coulson said both the drug and the by-product could be applicable for other neurodegenerative diseases, such as Alzheimer’s disease, or after a stroke.
“At this stage, the drug is a peptide and it is degraded by the body very quickly, but we’re actually really encouraged that something with such poor stability displayed real potential,” she said.
“I’ve been working on MND for almost 20 years and, if we can make this peptide stable and in the right drug form, we could be looking at an available treatment in two to 10 years.
“There are a lot of ‘ifs’ — one of which is that the drug might not work in humans with MND — but the mechanism of action revealed by the study, the way the drug works, should mean it could also be effective in Alzheimer’s and general dementia by promoting cognitive enhancement as well as slowing cell degeneration.”
In MND, neurons that control muscles for movement, speech and breathing undergo degeneration and die.
The average life expectancy following diagnosis with MND is 27 months.
The study is published in the Journal of Cell Science.
Media: QBI Communications, communications@qbi.uq.edu.au; Professor Elizabeth Coulson, e.coulson@uq.edu.au.





